By Dr. David J Tate – 02-05-2025
Endoscopic Submucosal Dissection (ESD) in the upper gastrointestinal tract is a demanding procedure, requiring not only technical dexterity but real-time recognition of subtle endoscopic signs. Among the most important of these is the Muscle Retraction Sign (MRS), a hallmark of potential deep submucosal invasion or challenging dissection planes. In this post, we explore a real-world case of ESD at the gastroesophageal junction (GEJ), where MRS was suspected and managed using meticulous technique and strategic planning.
What is the Muscle Retraction Sign?
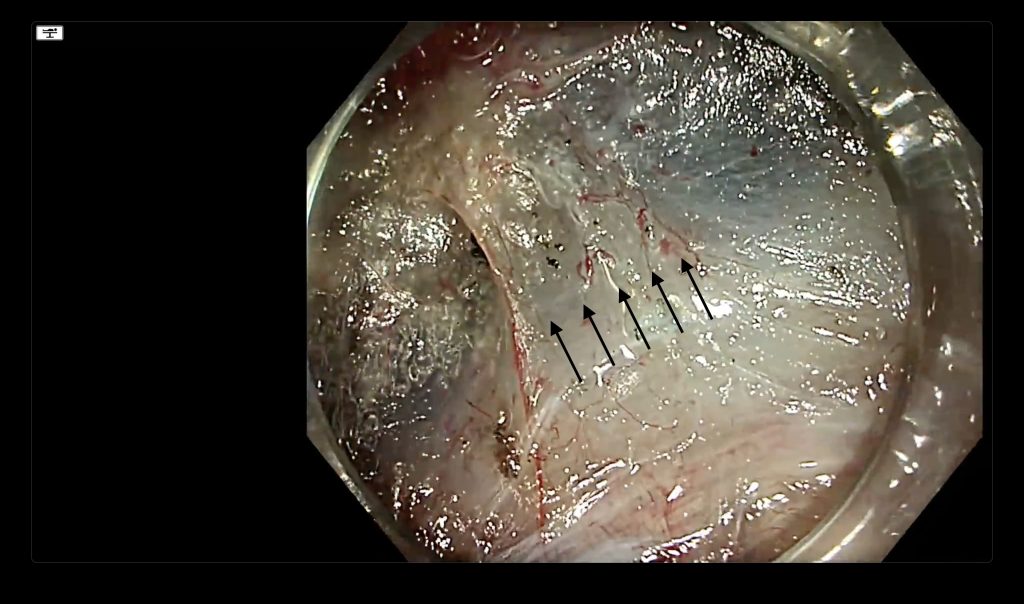
The Muscle Retraction Sign (MRS) appears during dissection as tenting or distortion of the muscularis propria toward the lesion. It often signals fibrosis, prior inflammation, or malignant infiltration. These features reduce the submucosal plane and increase the risk of deep margin involvement or even perforation if not managed carefully.
In the featured video, the endoscopist notes early signs of MRS—narrow submucosal space, tenting of the muscle, and proximity to key vascular structures:
“For me, this is risk of deep margin involvement… So we must work very, very carefully and precisely on the muscle layer close.”
How to Manage Suspected MRS: Technique and Strategy
1. Predict and Prepare: The endoscopist anticipates a complex resection and creates a submucosal pocket to access the lesion safely. The pocket offers a stable working environment and optimal scope control.
2. Visualize with Intent: Strategic insufflation and retroflexion are used to evaluate the lesion’s depth and exposure. The submucosal plane is carefully assessed for distortion.
3. Choose the Right Current: A precise SECT or cut mode is selected to reduce thermal spread and preserve the clarity of tissue layers. This is critical when working near distorted or ambiguous planes.
4. Bleeding Control: The team pre-coagulates large vessels with a low setting (e.g., Spray coagulation 0.5) to avoid bleeding artifacts. These artifacts could obscure the field and result in lost planes.
Clinical Decision-Making: When Not to Cut Deep
Despite visual cues suggesting deep invasion, the team opts against full-thickness resection to preserve surgical options, as the patient is fit for surgery:
“We could also decide to cut into the muscle here… but this patient is a surgically fit candidate, so we aren’t gonna do that here.”
This approach highlights a mature and conservative philosophy: mastery of ESD does not imply aggressive dissection at all costs. Instead, it prioritizes patient outcomes and oncological prudence.
Educational Takeaways
- Identify MRS early: Watch for narrowed planes, tented muscle, and vessel proximity.
- Plan your approach: Create a pocket and optimize working conditions before dissecting.
- Dissect with caution: Use current settings that limit scatter and respect tissue planes.
- Avoid bleeding at all costs: Pre-coagulate, isolate, and reassess regularly.
- Match the technique to the patient: Don’t jeopardize surgical options when curative surgical resection may be possible.
Watch the Full Video:
This video serves as a practical illustration of how theory translates into real-time decision-making in the ESD room. The MRS, once an abstract concept, becomes an actionable signal demanding precision, restraint, and thoughtful execution.
If you found this post helpful, consider subscribing for future clinical ESD tips and procedural walkthroughs.


